by MD Marc Mathieu · 2005 — Michel Brazier, MD, PhD1,2; Franck Grados, MD1; Said Kamel, PhD1,2;. Marc Mathieu, MD3; Alain Morel, BS1; Mohamed Maamer, PhD3;Jean-Luc Sebert, MD1;.
239 KB – 9 Pages
PAGE – 1 ============
Clinical and Laboratory Safety of One Year’s Use of a Combination Calcium + Vitamin D Tablet in Ambulatory Elderly Women with Vitamin D Insufficiency: Results of a Multicenter, Randomized, Double-Blind, Placebo-Controlled Study Michel Brazier, MD, PhD1,2; Franck Grados, MD1; Said Kamel, PhD1,2; Marc Mathieu, MD3; Alain Morel, BS1; Mohamed Maamer, PhD3;Jean-Luc Sebert, MD1; and Patrice Fardellone, MD, PhD 1 7Departments of Rheumatolo D, and Biochemistry, H6pital Nord, Amiens, France; 2Laboratory of Clinical Pharmacy, Bone Resorption Meckanisms Research Unit, INSERM ERI- 12, Pharmacy and Medicine Faculties, Amiens, France; and 31nnothera Laboratories, Arcueil, France ABSTRACT Objective: This article presents the results of an eval- uation of the clinical and laboratory safety of a 1-year course of treatment with a combination calcium and vitamin D tablet in ambulatory women aged >65 years with vitamin D insufficiency. Methods: In a multicenter, randomized, double- blind, placebo-controlled study conducted in France, women with a 25-hydroxyvitamin D level _<12 ng/mL were randomized to receive either a combination tablet containing calcium carbonate 500 mg and vitamin D 3 400 IU taken twice daily or a matching placebo tablet for 1 year. A complete clinical examination was per- formed at baseline and at 3, 6, 9, and 12 months of treatment; blood and urine samples were collected for laboratory analyses at the same time points. Safety was monitored based on adverse events recorded during the treatment period and on the results of laboratory tests, including measurement of creatinine and uric acid levels. Results: The study included 192 women (mean [SD] age, 74.6 [6.9] years; mean weight, 64.0 [12.5] kg), 95 in the calcium + vitamin D group and 97 in the placebo group. Fifty women (21/95 [22.1%] calcium + vitamin D, 29/96 [30.2%] placebo) were prematurely with- drawn from the study for various reasons, with no dif- ference in withdrawals between groups. Treatment- related adverse events were reported in 21 (22.1%) and 23 (24.0%) women in the respective treatment groups. These events consisted mainly of metabolic dis- orders (9 [9.5%] and 10 [10.4%], respectively), par- ticularly hypercalcemia (6 [6.3%] and 8 [8.3%]) and gastrointestinal disorders (9 [9.5%] and 8 [8.3%]). No major complications directly related to calcium and vitamin D supplementation occurred during the course of treatment. Although renal function was not altered, the group who received calcium + vitamin D had sig- nificantly elevated concentrations of serum uric acid compared with those who received placebo (52.3% vs 37.2%; P -- 0.046) but not urinary uric acid. Conclusions: In these ambulatory elderly women with vitamin D deficiency, supplementation with cal- cium + vitamin D appeared to be well tolerated over 1 year of treatment. No significant effects on creatinine clearance were observed. However, the proportion of women with elevated serum uric acid concentrations was significantly greater in those who received calci- um + vitamin D compared with those who received placebo. (Clin Ther. 2005;27:1885-1893) Copyright © 2005 Excerpta Medica, Inc. Key words: calcium, vitamin D, aged, women, long-term effects. INTRODUCTION Calcium and vitamin D are essential to bone health. Low calcium intake is one of the main risk factors for Accepted for publication October 3, 2005. doi: 10.1016/j.clinthera.2005.12.010 0149-2918/05/$19.00 Printed in the USA. Reproduction in whole or part is not permitted. Copyright © 2005 Excerpta Medica, Inc.
PAGE - 2 ============
osteoporosis, 1 and a lack of vitamin D can result in osteomalacia. 2 As a result of reduced exposure to ul- traviolet light (<2 hours/d) and/or inadequate dietary intake of vitamin D (<400 IU/d), -50% of women aged >65 years present with vitamin D insufficiency. 3,4 Osteoporosis and osteomalacia are associated with hip fracture, a major health problem among the elder- ly, particularly women, s-7 Long-term (1-3 years) supplementation with calci- um and vitamin D delays the development of osteo- porosis and prevents peripheral fractures in the elderly. 8-1° This antifracture effect is mediated mainly by an increase in bone mineral density 11 associated with a decrease in bone remodeling. 12 The prevalence of vitamin D insufficiency is well documented in France, as well as in countries at higher latitudes. 13,14 Linked to a lack of sun exposure, vitamin D insuffi- ciency is common in elderly institutionalized patients but can begin earlier in adulthood, with a positive northward geographic gradient. 13,14 Despite the fact that regular calcium and vitamin D supplementation is common among both elderly and younger popula- tions, a literature search identified few studies that focused on the long-term safety of such supplementa- tion. ls,16 In the study by Honkanen et al, 16 adminis- tration of calcium 1.558 g/d and vitamin D 1800 IU/d for 11 weeks in 25 independently living and 30 insti- tutionalized elderly women was associated with no adverse effects on safety indicators (serum calcium and creatinine). This article assesses the clinical and laboratory safety of a 1-year course of treatment with a combina- tion of calcium + vitamin D in ambulatory women aged >65 years with vitamin D insufficiency. Because of vitamin D’s mechanism of action–strong urinary excretion of calcium and correction of secondary hyperparathyroidism–particular attention was paid to renal function. PATIENTS AND METHODS Patients This study included community-dwelling ambula- tory women aged >65 years who spontaneously con- suited a practitioner and presented with vitamin D in- sufficiency (ie, serum 25-hydroxy vitamin D [25(OH)D] _<12 ng/mL). Exclusion criteria were hypercalcemia (serum calcium [sCa] >2.62 mmol/L), primary hyper- parathyroidism, renal insufficiency (serum creatinine [sCr] >130 pmol/L), or hepatic insufficiency. In addition, women who had received a bisphosphonate, calci- tonin, vitamin D or its metabolites, estrogen, raloxi- fene, fluoride, anticonvulsives, or any other treatment acting on bone metabolism (eg, glucocorticoids) in the past 6 months were excluded from the study. Each woman provided written informed consent before being included in the study. A local ethics com- mittee approved the protocol, and the trial was con- ducted in accordance with the Declaration of Helsinki, the Huriet law, and good clinical practice guidelines. Study Design This randomized, double-blind, placebo-controlled trial was conducted at 50 centers in 10 administrative regions throughout France. At each center, women were randomly allocated (4-block equilibrated randomiza- tion) to receive a single tablet* containing elemental calcium (calcium carbonate 500 mg) + vitamin D 3 (cholecalciferol 400 IU) or a placebo tablet twice daily for 1 year. The primary objective of the study was to assess the effects of treatment on bone mineral density and biochemical markers of bone formation and re- sorption. Its secondary objective was to evaluate the clinical and laboratory safety of treatment. This article presents the results of the safety evaluation. Immediately before their inclusion in the study, par- ticipants’ daily dietary calcium and vitamin D intakes were assessed using validated food-frequency question- naires. 17,18 Treatment compliance was assessed at each visit based on counts of the number of tablets taken compared with the number that was to be taken. Clinical Safety Assessment Clinical safety was evaluated in terms of sponta- neously reported and observed adverse events. The investigators assessed the causal relationship between each adverse event and study treatment. Adverse events leading to premature discontinuation and seri- ous adverse events were recorded, even if they were not considered possibly related to treatment. Hyper- calcemia (sCa >2.7 mmol/L), hypercreatininemia (sCr >130 pmol/L), and calcic lithiasis were considered ad- verse events and constituted cause for withdrawal from the study. All adverse events occurring during treatment were required to be reported immediately to a central site. *Trademark: Ideos ® (Innothera Laboratories, Arcueil, France).
PAGE – 3 ============
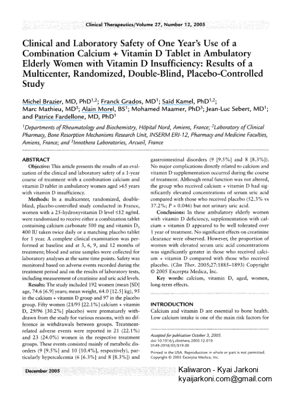
A complete clinical examination (height, weight, vital signs) was performed at baseline and at 3, 6, 9, and 12 months of treatment. Blood pressure was mea- sured using a sphygmomanometer on the dominant arm with the patient in a resting position. Grip strength in the dominant arm was measured using a dynamo- meter (Martin-Vigometer, Paris, France). Laboratory Safety Assessment The laboratory parameters focused on measures of renal function–sCr, urinary creatinine (uCr), serum uric acid (sUM, and urinary uric acid (uUA) levels. However, measures of calcium homeostasis were also assessed–serum 25(OH)D, intact parathyroid hor- mone (i-PTH), sCa, and urinary calcium (uCa) levels. Blood and urine samples were collected at baseline and after 3, 6, 9, and 12 months of treatment. Fasting blood samples were obtained by venipuncture. Serum was separated and frozen at -80°C until assayed. The previous day’s 24-hour urine samples were collected, frozen, and stored at -80°C until assayed. Serum 25(OH)D was measured using a competitive protein-binding assay after ethanol extraction fol- lowed by chromatographic purification. 19 Serum i-PTH was measured using an immunoluminometric assay (Magic Lite intact PTH, Ciba-Corning, Cergy Pontoise, France). sCa, sCr, and sUA were measured by colori- metric methods using an automated system (Ektachem 500 autoanalyzer, Johnson & Johnson, Rochester, New York). sCa was expressed as mmol/L (1 mmol/L = 4 mg/dL). Interassay reproducibility, expressed as per- cent coefficient of variation, was 10.8% for 25(OH)D and <2% for the other parameters, uCa, uCr, and uUA were measured in 24-hour samples. Calcium ex- cretion was expressed as the ratio of 24-hour uCa to uCr (uCa:uCr), and true creatinine clearance (CrC1) and uric acid clearance (UA C1) were calculated as 24-hour urinary flow x serum/urine concentration. These assays were performed by colorimetric methods using an automated system (Ektachem 500 autoana- lyzer). The interassay reproducibility, expressed as percent coefficient of variation, was <5%. Statistical Analysis Statistical analysis was carried out using SAS version 6.12 (SAS Institute Inc., Cary, North Carolina). The re- suits are expressed as numbers and percentages for qualitative variables, and as mean (SD), median, first quartile, and third quartile for quantitative variables. Medians were preferred to means in the case of nonnor- mal distribution (all laboratory values were considered to have nonnormal distribution). Comparisons between groups were performed using parametric tests (Student t test and ~2 test) and nonparametric tests (Wilcoxon signed-rank test and Wilcoxon rank sum test). The cor- relations between laboratory parameters were studied. Two-sided tests were performed with a type 1 error set at 5%. The study had 73% power to detect a significant difference in bone mineral density at L2-L4. The reference values for calcium homeostasis (25[OH]D, i-PTH, sCa, and uCa) had been determined previously in a similar population (women aged >65 years with vitamin D insufficiency), 2°,21 and values outside the normal range were defined by the usual upper or lower thresholds of the laboratory. Threshold values were as follows: 25(OH)D ___12 ng/mL; i-PTH >54 pg/mL; sCa >2.62 mmol/L; sUA >340 l~mol/L; sCr >130 l~mol/L; 24-hour uCa:uCr >6.25 mmol/ 24 hours; uUA >3.5 mmol/L; CrC1 <80 mL/min; and UA C1 <6 mL/min or >9 mL/min. RES U LTS Patient Population Of the 360 women recruited, approximately half were excluded from the study, mainly because baseline 25(OH)D levels were above the threshold of ___12 ng/mL for hypovitaminosis D (Figure). The study included 192 women who met all inclusion criteria, 95 in the group that received calcium + vitamin D and 97 in the group that received placebo (Table I). Baseline characteristics were comparable in the 2 study groups. Vitamin D and calcium intakes were low in both groups, usually lower than the recommended daily in- take (at least 200 IU/d and 1500 rag/d, respectively). Premature withdrawal occurred in 21 (22.1%) women who received calcium + vitamin D and 29 (30.2%) women who received placebo (n = 96 in the placebo group, as 1 woman did not receive at least 1 dose), with no difference in withdrawals between groups. The withdrawals were mainly the result of ad- verse events or the patient’s request. Compliance at each visit ranged from a median of 93.0% to 94.0% in the calcium + vitamin D group and from 93.0% to 96.5% in the placebo group. Global compliance was 92.0% in the calcium + vitamin D group and 92.5% in the placebo group. No signifi- cant difference in compliance was observed between the 2 groups at any visit. ~1887 :
PAGE – 4 ============
? .. i Recruited and assessed For eligibility i (N = 360) ! .. F” . { Excluded For Failure to meet i ->1 inclusion criterion (n = 168) . i Serum 25(OH)D >12 ng/mL (n = 154) {Serum calcium >2.62 mmol/L (n = 18) LAg e <.65 year___, s.(.n..- 5) Randomized i (n = 192) ! [- I L Calcium + vitamin D i (n = 9S) i . i II.,ILIIIII.// .. r Withdrawn (n = 21 [22.1%]) Adverse events (n = 15 [15.8%]) Gastrointestinal disorders (n = 3 [3.2%]) Cardiovascular disorders (n = 3 [3.2%]) Other (n = 9 [9.5%]) Patient's request (n = 9 [9.5%]) i Exclusion by investigator (n = 7 [7.4%]) :I Death (n = 3 [3.2%]) . --.c .. Analyzed (n = 95) Placebo i (n = 97) i i .. i W--t-hd iw in : 2; i;0:2%--ii; . Adverse events (n = 17 [17.7%]) Gastrointestinal disorders (n = 6 [6.3%]) Cardiovascular disorders (n = 4 [4.2%]) Other (n = 7 [7.2%]) Patient's request (n = 18 [18.8%]) Exclusion by investigator (n = 8 [8.3%]) Death (n = 1 [1.0%]) Analyzed I (n = 96) I Figure. Flow of subjects through the study. 25(OH)D = 25-hydroxyvitamin D. *One patient in the placebo group was withdrawn from the study before intake of the first dose and was excluded from analysis. Therefore, the percentages that follow were calculated based on 96 patients. Clinical Safety The number of adverse events overall was 187 in the calcium + vitamin D group and 170 in the place- bo group. There was no significant difference between groups in terms of the number of patients who ex- perienced _>1 adverse event (mean [SD], 69 [72.6%] calcium + vitamin D, 70 [72.9%] placebo), _>1 serious adverse event (14 [14.7%] and 12 [12.5%], respec- tively), _>1 adverse event leading to premature study discontinuation (15 [15.8%] and 17 [17.7%]), or _>1 adverse event possibly related to study treatment (21 [22.1%] and 23 [24.0%])(Table II). Adverse events leading to premature discontinua- tion mainly affected the gastrointestinal and cardio- vascular systems (Figure). Gastrointestinal adverse events in the calcium + vitamin D group included 2 cases of dyspepsia and 1 of abdominal pain; in the placebo group, there were 2 cases of nausea, 2 of gas- trointestinal bleeding, 1 of dyspepsia, and 1 of gas- tritis. Cardiovascular adverse events leading to pre- mature discontinuation in the calcium + vitamin D group included 2 cases of myocardial infarction and 1 case of stroke; in the placebo group, there were 2 cases of pulmonary edema, 1 of auricular fibrilla- tion, and I of stroke. Two women from the calcium + vitamin D group and none in the placebo group were withdrawn from the study because of hypercal- cemia. Three deaths occurred in the calcium + vita- min D group: a 93-year-old woman died suddenly at home, and a 91-year-old woman with angina pec- toris and a 71-year-old woman died of myocardial infarction. The latter patient had previously under-
PAGE – 5 ============
Table I. Baseline characteristics of study participants. Values are mean (SD), with the exception of laboratory pa- rameters, which are medians. Calcium + Vitamin D Placebo Overall Characteristic (n = 95) (n = 97) (N = 192) Age, y 74.2 (6.4) 75.0 (7.3) 74.6 (6.9) Weight, kg Body mass index, kg/m 2 Systolic blood pressure, mm Hg Diastolic blood pressure, mm Hg Heart rate, beats/min Grip strength (dominant hand), kPa Dietary calcium intake, mg/d Dietary vitamin D intake, IU/d Bone mineral density at L2-L4,* g/cm 2 Laboratory parametersf 25(OH)D, ng/mL i-PTH, pg/mL sCa, mmol/L sUA, #mol/L Creatinine, #mol/L uCa, mmol/24 h uUA, mmol/24 h CrCI, mL/min 65.2 (12.4) 62.8 (12.6) 64.0 (12.5) 27.0 (4.4) 26.4 (4.3) 26.7 (4.3) 138.5 (11.3) 138.0 (13.8) 138.3 (12.6) 77.9 (8.7) 77.1 (9.4) 77.5 (9.1) 72.4 (7.2) 72.7 (9.0) 72.6 (8.2) 63.6 (16.2) 62.3 (17.2) 62.9 (16.7) 751.7 (382.7) 720.8 (337.1) 736.0 (369.6) 84.9 (74.3) 83.9 (66.9) 84.4 (70.4) 0.937 (0.169) 0.889 (0.155) Not calculated 7.3 7.0 7.0 49 49 49 2.17 2.19 2.18 285 280 284 61 64 62 2.47 2.35 2.42 2.1 1.7 1.8 65.9 61.1 62.1 .. i 25(OH)D = 2S-hydroxy vitamin D; i-PTH = intact parathyroid hormone; sCa = serum calcium; sUA = serum uric acid; uCa = uri- nary calcium; uUA = urinary uric acid; CrCI = creatinine clearance, i *Numbers of patients in the respective treatment groups were 78 and 78 For this parameter. ! $Numbers of” patients in the respective treatment groups were 92 and 85 For these parameters, i gone gastrectomy for gastric neoplasia and had been hospitalized for severe psychiatric and gastric prob- lems probably resulting from cerebral metastasis. In the placebo group, a 91-year-old woman with angina pectoris presented with fatal acute pulmonary edema. All of these events were considered unrelated to treatment. In both groups, adverse events possi- bly related to study treatment were mainly metabol- ic and nutritional disorders (notably, hypercalcemia) or gastrointestinal disorders of mild or moderate intensity. No clinically significant changes in weight, blood pressure, heart rate, or grip strength were observed during the study. No major complications directly re- lated to calcium ÷ vitamin D supplementation oc- curred during the course of treatment. Laboratory Safety Laboratory values at the end of treatment are pre- sented in Table III. With regard to calcium homeo- stasis, after 1 year of treatment, >90% of wom- en in the calcium + vitamin D group had 25(OH)D levels above the threshold for hypovitaminosis D. Approximately 20% had high rates of uCa excre- tion, with a 24-hour uCa:uCr above the threshold value. The 24-hour uCa:uCr ratio was significant- ly higher in the calcium + vitamin D group compared with the placebo group (3.97 vs 2.35, respectively; P < 0.001) and serum i-PTH was significantly lower (31.0 vs 38.5 pg/mL; P < 0.001). Moreover, the median i-PTH value was within the normal range (31 pg/mL) in the calcium + vitamin D group. These changes in calcium homeostasis had no effect on cal-
PAGE - 6 ============
Table II. Number (%) of women with _>1 adverse event during the study. Calcium + Vitamin D Placebo Category (n = 95) (n = 96*) P ! No. of women with _>1 adverse event 69 (72.6) 70 (72.9) 1.00 Specific adverse events, by body system Osteom uscular Gastrointestinal Metabolic and nutritional Hypercalcemia Serious adverse events, by body system Cardiovascular Osteomuscular Nervous Gastrointestinal Body as a whole Other* Adverse events judged possibly treatment related Metabolic and nutritional Hypercalcemia Gastrointestinal 32 (33.7) 24 (25.0) 0.21 22 (23.2) 21 (21.9) 0.86 16(16.8) 18(18.8) 0.85 7 (7.4) 11 (11.5) – 14 (14.7) 12 (12.5) 0.68 6 (6.3) 5 (5.2) 0.62-1.00f 5(5.3) 2(2.1) 0.27 1 (1.1) 2 (2.1) 1.00 1 (1.1) 2 (2.1) 1.00 1 (1.1) 1 (1.1) 1.00 2 (2.1) 3 (3.2) 0.50-1.00t 21 (22.1) 23 (24.0) 0.86 9 (9.5) 10 (10.4) 1.00 6(6.3) 8(8.3) – 9(9.5) 8(8.3) 0.81 *One subject was withdrawn from the study before receiving the first dose of study medication and was excluded from analysis. tStatistical analyses (X 2 test) were performed separately for general cardiovascular, cardiac, and vascular disorders. For the “other” category, statistical analyses were performed by body system. *The other serious adverse events were malaria, infection, uterovaginal prolapse, and hemorrhage. cemia, which did not differ between the 2 groups (2.29 and 2.19 mmol/L). With regard to renal function, there was no signifi- cant difference in uUA between the calcium + vitamin D group and the placebo group (1.9 mmol/24 hours in both groups). A significantly greater number of pa- tients in the calcium + vitamin D group had sUA lev- els above the normal threshold (52.3% calcium + vitamin D vs 37.2% placebo; P = 0.046), but without any changes in UA C1. There were no significant changes in creatinine metabolism. The relationships between baseline laboratory val- ues for the overall study population and on-treatment values for the calcium + vitamin D group (all study data pooled) were analyzed. The baseline values illus- trated the known positive correlation between 25(OH)D and 24-hour uCa:uCr (r = 0.19; P < 0.001) and the negative correlation between i-PTH and both the 24-hour uCa:uCr (r = -0.13; P = 0.016) and 25(OH)D (r = -0.24; P < 0.001). Moreover, sUA was strongly correlated with the calcium homeostasis pa- rameters 25[OH]D, i-PTH, and 24-hour uCa:uCr (25[OH]Dr r = 0.2, P = 0.005; i-PTH: r = 0.2, P = 0.004; 24-hour uCa:uCr: r = -0.25, P < 0.001), particularly with the latter. Similar results were reported for UA C1 (25[OH]Dr r = 0.24, P < 0.004; i-PTH: r = -0.02, P = 0.006; 24-hour uCa:uCr: r = 0.5, P < 0.001), whereas uUA was correlated only with 25(OH)D (r = 0.3, P = 0.007) and 24-hour uCa:uCr (r -- 0.49, P < 0.001). CrCI was correlated only with 24-hour uCa:uCr (r = 0.55, P < 0.001). After 1 year of treatment with calci- um + vitamin D, only 24-hour uCa:uCr was correlated with uric acid parameters (sUA: r = -0.16, P = 0.007; uUA: r -- 0.54, P < 0.001; UA Ch r = 0.56, P < 0.001). DISCUSSION In this 1-year, double-blind, prospective study in a large population of ambulatory elderly women with vita- min D insufficiency and normal renal function, com- bined calcium and vitamin D treatment was well tolerated. It is well known that long-term oral admin- istration of appropriate doses of this combination can simultaneously produce marked increases in 25(OH)D and uCa levels and a decrease in i-PTH levels, reflect-
PAGE - 8 ============
curring with a similar incidence in both groups. Three deaths occurred in the calcium + vitamin D group and 1 in the placebo group, none of them considered pos- sibly related to study treatment. In terms of changes in laboratory parameters, no significant difference in sCa was observed between the 2 groups. There were several cases of hypercalcemia, with no statistical difference between groups. Two women in the calcium + vitamin D group were with- drawn from the study due to hypercalcemia. It has been reported that calcium therapy may cause hyper- calcemia in those with conditions such as chronic renal disease29; women with chronic renal failure, however, were excluded from this study. Moreover, vitamin D is potentially toxic: hypercalciuria, hypercalcemia, and an increase in creatinine levels have been reported with vitamin D therapy at doses 20 to 30 times phys- iologic levels. 3° Vitamin D at a dosage of 2000 IU/d for 6 months produced hypercalcemia in an elderly population, 31 and dosages <2000 IU/d may also cause hypercalcemia in these patients, suggesting an in- creased susceptibility to the action of vitamin D. 3° Given the potential renal toxicity of calcium + vitamin D therapy, this study focused on measures of renal func- tion, particularly uric acid metabolism. At baseline, a significant correlation was found between uCa on the one hand and sUA, uUA, UA C1, and CrC1 on the other (all, P < 0.001). After 1 year of treatment, this relation- ship persisted only for parameters of uric acid metabo- lism. Such a relationship has been reported in patients with primary hyperparathyroidism, with a positive cor- relation between 24-hour uCa:uCr and 24-hour uUA:uCr, suggesting a possible relationship between the metabolism of calcium and uric acid. 32 Moreover, a positive correlation has been found between serum lev- els of 1.25(OH)2D, the active metabolite of vitamin D, and uUA and uCa in patients who form calcium stones. 33 Therefore, the fact that significantly more women in the calcium + vitamin D group than in the placebo group had elevations in sUA (P = 0.046) in the present study must be taken into consideration. However, long-term administration of calcium + vitamin D did not lead to any significant change in creatinine levels. It may be necessary to monitor levels of sUA during long-term supplementation with calcium + vitamin D. CONCLUSIONS In these ambulatory elderly women with vitamin D deficiency, supplementation with calcium + vitamin D appeared to be well tolerated over 1 year of treatment. No significant effects on CrC1 were observed. However, the proportion of women with elevated sUA concen- trations was significantly greater in those who re- ceived calcium + vitamin D compared with those who received placebo. ACKNOWLEDGM ENTS This study was supported by Innothera Laboratories, Arcueil, France. The authors thank Fabienne Peretz for assistance with the writing of this article and the PREDOS Asso- ciation, Amiens, France, particularly Fabienne Hervy, for technical assistance. REFERENCES 1. OmdahlJL, Garry PJ, Hunsaker I_A, et al. Nutritional sta- tus in a healthy elderly population: Vitamin D. AmJ Clin Nutr. 1982;36:1225-1233. 2. Nordin BE, Heyburn PJ, Peacock M, et al. Osteoporosis and osteomalacia. Clin Endocrinol Metab. 1980,9:177-205. 3. Gloth FM III, TobinJD. Vitamin D deficiency in older peo- ple.JAm Geriatr Soc. 1995;43:822-828. 4. Prince RL, Dick I, Devine A, et al. The effects of meno- pause and age on calcitropic hormones: A cross-sectional study of 655 healthy women aged 35 to 90.J Bone Miner Res. 1995;10:835-842. 5. Aaron]E, GaHagherJC, Anderson J, et al. Frequency ofos- teomalacia and osteoporosis in fractures of the proximal femur. Lancet. 1974;1:229-233. 6. Greenspan SL, Maitland LA, Myers ER, et al. Femoral bone loss progresses with age: A longitudinal study in women over age 65. J Bane Miner Res. 1994;9:1959-1965. 7. Ensrud KE, Palermo L, Black DM, et al. Hip and calcaneal bone loss increase with advancing age: Longitudinal re- sults from the study ofosteoporotic fractures.J Bone Miner Res. 1995;10:1778-1787. 8. Riis B, Thomsen K, Christiansen C. Does calcium supple- mentation prevent postmenopausal bone loss? A double- blind, controlled clinical study. N EnglJ Med. 1987;316: 1 73-177. 9. Chapuy MC, Chapuy P, Meunier PJ. Calcium and vitamin D supplements: Effects on calcium metabolism in elderly people. AmJ Clin Nutr. 1987;46:324-328. 10. Dawson-Hughes B, Harris SS, Krall EA, Dallal GE. Effect of calcium and vitamin D supplementation on bone den- sity in men and women 65 years of age or older. NEnglJ Med. 1997;337:670-676. 11. Christiansen C, Christensen MS, McNair P, et al. Prevention of early postmenopausal bone loss: Controlled 2-year study in 315 normal females. EurJ Clin Invest. 1980; 10:273-279.
PAGE - 9 ============
12. Brazier M, Kamel S, Maamer M, et al. Markers of bone remodeling in the elderly subject: Effects of vita- min D insufficiency and its correc- tion. J Bone Miner Res. 1995;10: 1753-1761. 13. Fardellone P, SebertJL, Garabedian M, et al. Prevalence and biological consequences of vitamin D deficien- cy in elderly institutionalized subjects. Rev Rhum Engl Ed. 1995;62:576-581. 14. Chapuy MC, Preziosi P, Maamer M, et al. Prevalence of vitamin D insuf- ficiency in an adult normal popula- tion. Osteoporos Int. 1997;7:439-443. 15. McKenna MJ, Freaney R, Byrne P, et al. Safety and efficacy of increasing wintertime vitamin D and calcium intake by milk fortification. QJM. 1995;88:895-898. 16. Honkanen R, Alhava E, Parviainen M, et al. The necessity and safety of calcium and vitamin D in the elder- ly.JAm Geriatr Soc. 1990;38:862-866. 17. Fardellone P, SebertJL, Bouraya M, et al. Evaluation of the calcium content of diet by frequential self- questionnaire [in French]. Rev Rhum Mal Osteoartic. 1991 ;58:99-103. 18. Grados F, Brazier M, Kamel S, et al. Effects on bone mineral density of calcium and vitamin D supplemen- tation in elderlywomen with vitamin D deficiency. Joint Bone Spine. 2003; 70:203-208. 19. Zeghoud F, Jardel A, Guillozo H, et al. 25-Hydroxyvitamin D: Develop- ment ofa microassay by radiocompe- tition. Pediatric interest [in French]. Immunoanal Biol Spec. 1991;27:29- 33. 20. Kamel S, Fardellone P, Meddah B, et al. Response of several markers of bone collagen degradation to calci- um supplementation in postmenopaus- al women with low calcium intake. Clin Chem. 1998;44:1437-1442. 21. Fardellone P, Brazier M, Kamel S, et al. Biochemical effects of calcium supplementation in postmeno- pausal women: Influence of dietary calcium intake. AmJ Clin Nutr. 1998; 67:1273-1278. 22. Krall EA, Sahyoun N, Tannenbaum S, et al. Effect of vitamin D intake on seasonal variations in parathyroid hormone secretion in postmeno- pausal women. N EnglJ Med. 1989; 321:1777-1783. 23. Woitge HW, Knothe A, Witte K, et al. Circaannual rhythms and inter- actions of vitamin D metabolites, parathyroid hormone, and bio- chemical markers of skeletal homeo- stasis: A prospective study. J Bone Miner Res. 2000;15:2443-2450. 24. Chapuy MC, Arlot ME, Delmas PD, Meunier PJ. Effect of calcium and cholecalciFerol treatment for three years on hip fractures in elderly women. BMJ. 1994;308:1081-1082. 25. Lamberg-Allardt CJ, Outila TA, Karkkainen MU, etal. Vitamin D de- ficiency and bone health in healthy adults in Finland: Could this be a concern in other parts of Europe? J Bone MinerRes. 2001 ;16:2066-2073. 26. NIH Consensus Conference. Optimal calcium intake. NIH Consensus De- velopment Panel on Optimal Calcium Intake.JAMA. 1994;272:1942-1948. 27. Larsen ER, Mosekilde L, Foldspang A. Vitamin D and calcium supple- mentation prevents osteoporotic Fractures in elderly community dwelling residence: A pragmatic population-based 3-year interven- tion study. J Bone Miner Res. 2004; 19:370-378. 28. Riggs BL, O'Fallon WM, Muhs J, et al. Long-term effects oFcalcium sup- plementation on serum parathyroid hormone secretion level, bone turn- over, and bone loss in elderly wom- en. J Bone Miner Res. 1998;13:168- 174. 29. Riggs BL, Seeman E, Hodgson SF, et al. EFFect of fluoride/calcium regimen on vertebral Fracture occurrence in postmenopausal osteoporosis. Com- parison with conventional therapy. N EnglJ Med. 1982;306:446-450. 30. Parfitt AM, Gallagher JC, Heaney RP, et al. Vitamin D and bone health in the elderly. AmJ Clin Nutr. 1982; 36(Suppl 5):1014-1031. 31. Johnson KR, Jobber J, Stanawski SW. Prophylactic vitamin D in the elderly. Age Ageing. 1980;9:121-127. 32. Yamamoto S, Hiraishi K, Nakamura S, Ghazizadeh M. Serum and uri- nary uric acid in primary hyperpara- thyroidism. BrJ Urol. 1987;59:386- 389. 33. Jarrar K, Amasheh RA, Graef V, Weidner W. Relationship between 1,25-dihydroxyvitamin-D, calcium and uric acid in urinary stone Form- ers. Urollnt. 1996;56:16-20. Address correspondence to: Professor Patrice Fardellone, Service de Rhumatologie, H6pital Nord, 80054 Amiens Cedex 1, France. E-maih fardellone.patrice@chu-amiens.fr The author has requested enhancement of the downloaded file. All in-text references underlined in blue are linked to publications on ResearchGate.The author has requested enhancement of the downloaded file. All in-text references underlined in blue are linked to publications on ResearchGate.
239 KB – 9 Pages